Renew-Bloom-Flourish
There Is A Reason Why Current Medications Don't Work Well.
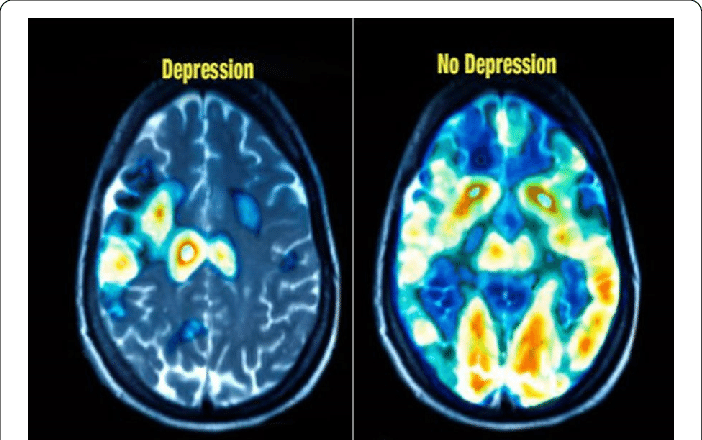
If your current prescription medications are falling short, recent discoveries in brain imaging studies reveal a new treatment and why it might help.
Medications are a standard and sometimes an effective treatment for depression, migraines, and Fibromyalgia, but they are far from perfect. In fact, in some cases, our current medications have proven to be no better than a sugar pill or placebo, and some patients don't respond to any current drug options.
I've Tried Everything And... Nothing Works!
Even after over 50 years of medical research, prescription medications have not been very effective in treating most people suffering from depression, migraines, Fibromyalgia, and other forms of chronic pain. These limited treatment options represent a vast clinical challenge, and many people continue to struggle.
From the time drugs were first developed back in the 1950s to today, they have all worked through similar biochemical actions. The most commonly known and prescribed class of drugs is the selective serotonin reuptake inhibitor, or "SSRI." These drugs, including Prozac, Zoloft, Paxil, and Lexapro, attempt to regulate the amount of serotonin, a brain chemical called a neurotransmitter that carries signals between neurons and thought to control mood. The assumption is that if you could increase the amount of serotonin (or dopamine or norepinephrine) available, your symptoms would improve.
Unfortunately, they have not been as helpful as we had hoped for many people. And the response rate to them is not as high as we need it to be. Studies have shown that only 1 in 3 patients respond to any single SSRI, and if they do respond, it can take several weeks or months before experiencing improvement. Even more aggressive new treatments to combat mood disorders, such as transcranial magnetic stimulation (rTMS), are only about 38% effective, and even the older "gold standard" treatment of psychiatry, electroconvulsive shock treatment (ECT), is not much better. It is only effective for about 50% of patients. At the same time, Deep TMS (Brainsway) has shown success rates of up to 65% it doesn’t always work for everybody.
Why Haven't We Been Able To Do Better?
Until now, treatments for depression with antidepressants assumed that low levels of brain neurotransmitters like serotonin and dopamine were the cause of depression. But what if we were wrong? The answer to that question may become apparent with new cutting-edge research and brain imaging studies showing how the brain works.
Significant findings emerged in the late 1990s with the observation by researchers that brain tissue in critical areas of the brain was reduced in people who had been under prolonged stress and in combat veterans who had developed depression and PTSD.
Investigators at Stanford University suggested that stress might cause the "death" of neurons, suggesting that the critical brain size reductions seen in patients under stress and those with depression and PTSD might reflect the loss of nerve cells.
These new findings suggest that the old theory about low serotonin causing these illnesses may be incorrect. But why were these vital areas of the brain "shrinking" and getting smaller and smaller?
The "Disconnected" Brain
The answer to that question was found with the development of a new type of MRI study called Diffusion Tensor Imaging or "DTI." Researchers could use DTI techniques to examine these areas and the "neural network connections" around them in much greater detail.
With this new way to look at the brain's inner workings, it became apparent that these critical neural circuits, which play an essential role in the development of major depressive disorders, Fibromyalgia, and even migraine headaches, were becoming "disconnected" and isolated in some way.
They saw microscopic changes occurring between the white matter (wiring-neural circuit pathways) of the higher and deeper layer of the brain known as the cortical-subcortical circuits, leading to a type of "disconnection syndrome" between those regions. This decrease in "connectivity" linking the various critical areas of the brain appears to be directly involved in developing multiple disorders, including depression, anxiety, and PTSD.
The loss of these connections means that various areas of the brain may no longer communicate information effectively and become stuck in a sort of continuous "loop." Almost like a computer program that freezes and won't work correctly. It now appears that this "disconnection" in the brain's wiring network and loss of communication is responsible for low neurotransmitters levels.
The repetitive circuits may only communicate limited signals, like continuous thoughts and feelings of depression, anxiety, or pain, by losing those connections. We now suspect that as these critical connections are lost or "disconnected," people may feel depressed, anxious, or start to experience pain, increased sensitivity, and headaches. Often they also report having difficulty concentrating or remembering important information. The result is that everyday life can become challenging and less meaningful. Friends, family, and things they used to enjoy no longer seem to please them.
It can seem almost as if someone has slowly and methodically "turned off" all the light switches in a big house, and now the house becomes cold, uncomfortable, dark, and gloomy.
If that is the case, the question then becomes; can you restore those lost connections?
New Options to "Reboot and Reconnect" the Brain
New research shows additional evidence supporting the "disconnection syndrome" theory and suggests that the connections can be "restored or rebooted."
Part of that research was discovering that a 50-year-old medication commonly used for anesthesia can have some remarkable "side effects." Researchers were astonished when they discovered that following the intravenous administration of ketamine, they saw a rapid "reconnection" of the brain network. More than that, they found that brand-new nerve connections began to develop almost immediately following treatment.
Dendritic spine remodeling. Images taken at baseline, after chronic stress, and after a single dose of ketamine. Red arrows point to eliminated spines; blue arrows to new spines.
Ketamine was found to have this unusual effect by stimulating a brain "nerve growth" factor known as BDNF, which could reverse some of the disconnections in minutes. That small study conducted at Yale also established an arbitrary "standard" for ketamine infusions in the treatment of mood disorders. To this day, the standard was, and is, "administer 0.5mg/kg of ketamine over 40 minutes" based on body weight.
While the effects of ketamine were astounding, and it was truly remarkable that the brain could be "reconnected" so quickly, there was a catch. After a single infusion, the "rebooting" only lasted 3-7 days before the connections were lost and symptoms returned.
How could it be made to last longer?
o study this, one group in Minnesota and another in New York thought that ketamine might work like another older and more aggressive form of therapy known as electroconvulsive therapy or "ECT." They knew that it usually requires six or more ECT sessions before a person improves, so perhaps ketamine needed to be given more than once, just like ECT.
To test this hypothesis, they began to administer six ketamine infusions, one every other day for two weeks, just like they would for ECT. What they found by doing that was that the improvement seen could be extended to 1 month before the patients needed another infusion. That was better than 3-7 days, but patients continued to need ongoing "booster infusions" every four weeks after that to make it last.
While six infusions given every other day for two weeks did improve the benefits of ketamine substantially, many patients found it challenging to return each month for "boosters." We thought it could be better, and it was always a little surprising that few have had the imagination, experience, or expertise administering ketamine infusions to improve on it.
Since then, others have adopted that same protocol without realizing or understanding that it was not intended to treat depression, nor was it optimized to achieve the most effective serum concentrations necessary. So, today the only factor that many physicians and "ketamine clinics" consider when determining your infusion is your body weight. They rely upon a simple, straightforward formula of "so many milligrams" of ketamine per kilogram of your weight and administer the infusion over 40 minutes.
Using that approach, the results today are about the same as they were almost 20 years ago. Approximately 70% of research-study patients will show improvement, while only about 40-50%. "Real-world" patients treated in a community ketamine practice will have a 50% or better reduction in their symptoms for about one month before requiring another infusion to maintain the benefits. Still, even with the need for six infusions to have the effects last one month, the effectiveness of this approach is far better than those obtained for many with conventional antidepressant therapy.
Although Dr. Grass was initially impressed with the results, it was also clear that many other factors could influence how well the infusion worked. After all, we all have taken either over-the-counter or prescription medications at one time or another; and most medications come in various strengths for different conditions. For example, Prozac, an older and common antidepressant, is supplied in 10mg, 20mg, 40mg, and 90mg strengths. It is available in multiple doses because each person will metabolize the drug differently, some more slowly and others very rapidly, leading to different amounts of the medication in their system. Some conditions may be more challenging to treat and require more medicine to be effective. Also, there may be potential drug interactions to consider. Whenever we start a new medication, our practitioner or pharmacist will warn us about taking other medicines simultaneously and how they might negatively interact. The same is also true for ketamine.
So, based on common sense and logic, there was room for improvement with ketamine infusions utilizing the same approach. The first step was to determine if other doses or specific serum concentrations of ketamine would be more effective or last longer. Once that was determined, the next step was determining the time necessary to maintain that concentration for each person to have a maximal effect. Finally, what other metabolic or medication issues affect how well someone would respond or how long the improvements would last?
Dr. Grass knew we had to look at this in a new way to get the best results, so we took a different approach. Some people think all people with illnesses like depression, fibromyalgia, or migraines are alike. With that thinking, you give the same medication, in the same amount, to everyone in the same way and hope they improve. Unfortunately, as we all know, it doesn't always work well that way.
But we knew that each person is unique and different, so it was apparent that the treatment must be individually tailored to match the patient. Rather than use an old model like ECT, we used a new integrated and systems model. Using the same old methods and expecting different results never leads to breakthroughs.
There were many factors to consider. To begin, the amount of medication needed from patient to patient can vary greatly. Based on our experience, we knew that it was critically important to achieving a certain "blood level" or effective serum concentration, also known as the effective dose for 95% of patients or (ED95), to achieve optimal results. This can be challenging, and many physicians are unaware of the optimal serum concentrations needed.
But there was even more than that to consider. Precision Medicine and innovative clinical research have shown a wide variation in the way people metabolize medications, which is often due to liver enzymes known as Cytochrome P450. More than that, some individuals may lack acetyl-L-carnitine (LAC) or have a BDNF variant which may affect optimal treatment response. It is also vitally important to account for other factors such as current medications, metabolism, body composition, ancestral heritage, and genetic factors, which all play a critical role in treatment response. All of these factors need to be considered to have the best result.
And then, Dr. Grass found that it was essential to optimize the amount of medication given, and we had to change how it was administered. It had to be carefully adjusted to each patient, minute-by-minute, while constantly monitoring them and adding synergistic agents; if all of that was done carefully, then ketamine worked remarkably better and lasted much longer. Following this approach, he discovered we could achieve better results with reduced overall infusions required.
Over seven years, Dr. Grass could identify and determine optimal levels, the time necessary to maintain them, and what effect body metabolism and other medications had on the infusion. For example, to have predictable and consistent results, body mass composition, not total body weight, directly affects the serum concentration of ketamine achieved during an infusion. Also, Dr. Grass found that a person's basic metabolic rate for drugs, current medications, hormones, and carnitine levels all affect the response to ketamine. So, before we consider beginning an infusion, we spend a great deal of time determining if each patient is in an optimal state to have an infusion or requires specific additional lab tests or supplementation before beginning infusion therapy to have the best results.
Although the Flourish Infusion takes more work to work up, target, and give, the results lead to higher outcomes for our clients. Contact us and see why Iris Ketamine and Infusions should be your first choice for ketamine care in Indiana.
Renew-Bloom-Flourish
"It’s a scary thing trying to get help, but Iris took a lot of that anxiety and fear out of the equation. I got targeted treatment which I know made all the difference."
— Ray, Iris Ketamine Client
FAQs
Where should I start?
The first step in your journey should be finding a trained and qualified provider to administer ketamine infusions safely and effectively, according to the American Psychiatric Association and the American Society of Anesthesiologists guidelines.
"Ketamine Clinics" are becoming more common in some communities and, unfortunately, can vary widely in quality, experience, and expertise. Some providers providing ketamine infusion therapy may be well-meaning but have little knowledge or formal training in ketamine infusion therapy. They frequently hear about the remarkable benefits of ketamine for depression and anxiety, read one or two papers published on the subject, and then think they are qualified to begin performing infusions. Because of this, results can vary widely, and many patients do not achieve the full benefits of ketamine therapy.
Ketamine therapy is an exact and meticulous therapy that requires experience and expertise. Unfortunately, some providers may see ketamine infusion therapy as a simple office procedure requiring little or no direct involvement and can produce additional revenue for their practice. They often see other patients while a nurse starts your infusion in an isolated exam room and occasionally "checks in on you."
In our view and the opinion of the American Psychiatric Association, this is not a safe practice. Let's not forget that ketamine is a potent medication, and it is an anesthetic drug. You should be very cautious if the provider is only with you for five minutes before the infusion or if a fully trained healthcare team member is not with you at all times during your infusion.
What should I be looking for?
1. Be very skeptical of any "ketamine clinic" that uses a "call-in" answering service to give you information. You will often speak to someone in a remote location with no personal knowledge of ketamine therapy, which can only answer simple questions from a script. They may only be concerned with offering you an appointment in the clinic as soon as possible. It would help if you spoke to someone with direct knowledge and experience in ketamine infusion therapy who can answer all your questions.
2. Ask where they were trained in the use of ketamine. Your provider should be thoroughly trained and experienced in administering ketamine for mood disorders and related conditions. Ask if they are certified in ketamine therapy. The Ketamine Research Institute trains providers from around the US and Internationally to administer ketamine safely under strict protocols and guidelines set forth by the American Psychiatric Association and the American Society of Anesthesiologists recommendations.
3. Be very careful if they do not assure you that a fully qualified healthcare team member will always be with you during the infusion session. It is not advisable to have someone from the office "check in on you" occasionally. You are given a potent medication that should be observed and monitored continually during your treatment.
4. Be suspicious of any provider that prescribes supplemental ketamine in a nasal spray or oral formulation. There are many unintended consequences to using such agents, including the possibility of having adverse side effects, becoming dependent, or developing tolerance to the medication quickly and thereby losing its effect rapidly. Ketamine should always be administered under the care and safety of a healthcare professional.
5. Be concerned if they do not require your medical records. All legitimate providers providing ketamine to a patient will request medical records and labs from your doctor. If they do not ask for these documents or say they are unnecessary, that may be a warning sign that they may not be reputable and are operating a "mill" type of operation.
What can the Flourish protocol treat?
Depression Migraine Headaches
Generalized Anxiety Bipolar Disorder
Post Traumatic Stress Disorder
And More!